Femoroacetabular Impingement (FAI): a common but neglected cause of hip pain!
- Ajinkya Achalare
- Aug 13, 2025
- 4 min read
Ever faced a momentary sharp pain in your groin region while playing sports or getting down from a car?
Hip or groin pain is relatively rare complaint among athletes and middle-aged individuals who lead an active life. One of the frequently overlooked causes of persistent hip discomfort in this age group is FemoroAcetabular Impingement (FAI).
This condition, if ignored over a long period, can lead to progressive hip damage, reduced mobility, and even early-onset arthritis of the joint. However, with early diagnosis and appropriate treatment, it is possible to restore hip function and return to an active lifestyle.
Let’s try to understand what this entity is really about.
What is FAI?
Femoroacetabular Impingement (FAI) is a condition where abnormal contact occurs between the femoral head (the ball of the thigh bone) and the acetabulum (the hip socket) due to changes in their bony architecture. This repetitive friction leads to pain, limited hip movement, and damage to the cartilage and labrum.
The hip joint is designed for smooth, pain-free movement. In FAI, bony irregularities disrupt this harmony, resulting in mechanical irregularity during activities like squatting, running, twisting, or even prolonged sitting.
What are the types of FAI?

It can be classified into three main types:
1. Cam Impingement:
In this type, the femoral head is not perfectly round.
The abnormal bone shape causes it to jam into the acetabulum during movement.
This is more common in young athletes, particularly males, who engage in sports requiring repetitive hip flexion and rotation.
2. Pincer Impingement:
Here the acetabulum (socket) has excess bone leading to over-coverage of the femoral head.
This causes the labrum (soft boundary tissue) to be pinched between the bones, resulting in pain and gradual tear in it.
Pincer impingement is more commonly seen in middle-aged women.
3. Combined (Mixed) Impingement:
Many patients have features of both cam and pincer impingement.
This combination further increases the risk of hip joint damage if not addressed early.
Who is likely to develop FAI?
FAI is generally caused by subtle changes in hip anatomy. These changes may develop during growth or result from repetitive stress over time. Common causes and risk factors include:
Genetic predisposition: Some individuals are born with slight anatomical differences that make impingement more likely.
High-impact sports: Activities such as football, hockey, basketball, dancing, which involve frequent hip rotation and deep flexion, increase the risk.
Repetitive stress injuries: Continuous micro trauma to the hip joint can accelerate bony overgrowth.
Developmental conditions: Conditions like slipped capital femoral epiphysis (SCFE) or Legg-Calvé-Perthes disease during childhood may predispose an individual to develop FAI later in life.
How can you tell if you have FAI?
FAI symptoms can develop gradually and are often mistaken for simple muscle strain. The hallmark signs include:

Groin pain: It is the most common symptom, often deep and aching, worsens with activity, squatting, and sitting cross-legged.
Hip stiffness: Difficulty in bending or rotating the hip, especially during sports or everyday movements.
Clicking or locking: A sensation of catching or clicking in the hip joint due to labral tears.
Pain becomes more severe, persistent and progressive once the arthritis starts to set in.
How is it diagnosed?

Physical examination: The doctor checks range of hip movements, strength, and impingement signs through specific tests.
X-rays: These help to visualise the shape of the hip bones and detect cam or pincer deformities and quantify them by drawing some angles. In most of the cases, X-rays are confirmatory for FAI.
MRI: May be required to know the status of the labrum
CT scan: In some cases, it is used for 3D visualisation before surgical planning.
What are the treatment options available?
Treatment depends on the severity of the condition, the level of hip damage, and the patient’s functional demands.
1. Non-Surgical Management:
These are preferred in mild cases with short history, without significant deformity.
Activity modification: Avoiding deep squats, twisting movements or prolonged sitting can reduce symptoms.
Physical therapy: Targeted exercises help improve hip strength, flexibility, and joint biomechanics. Strengthening the core and gluteal muscles helps relieving the stress on the hip.
Medications: Non-steroidal anti-inflammatory drugs (NSAIDs) help control pain and inflammation in acute stages
Injections: Corticosteroid or platelet-rich plasma (PRP) injections can provide temporary relief in some cases, where oral medications don’t help.
2. Surgical Management
If conservative treatment fails or if there is significant labral damage, hip arthroscopy is the way forward.
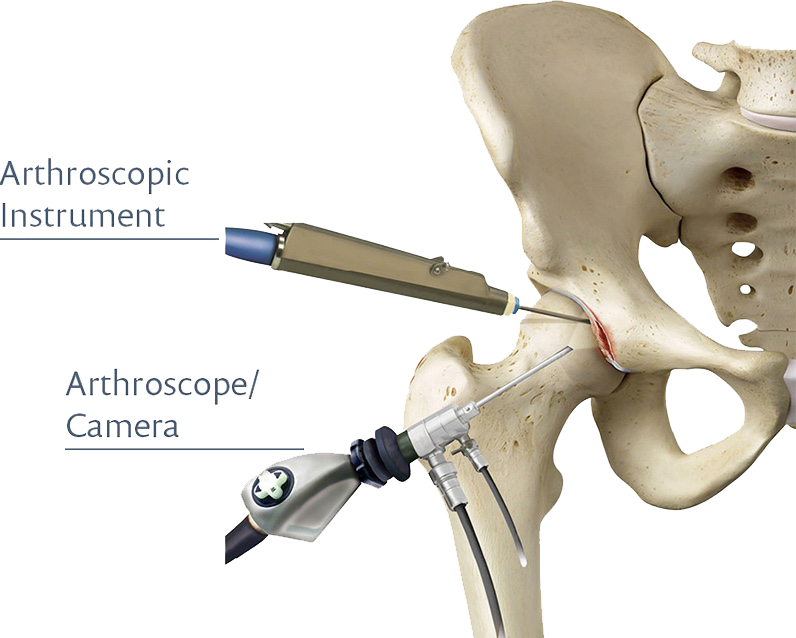
Hip arthroscopy: It is a minimally invasive key-hole surgical procedure which offers maximum benefits in deep-seated joints such as the hip. Through this procedure, the deformed bones are reshaped, and the torn labrum is repaired or reconstructed.
Timely surgical intervention can prevent the progression to hip arthritis and preserve the joint.
FAI can not be prevented but hip arthritis can be!
Early diagnosis and management can significantly reduce long-term complications:
Pay attention to subtle hip or groin pain.
Avoid repetitive movements that aggravate symptoms.
Engage in hip-strengthening and mobility exercises. Consult a physiotherapist to help you.
Consult an orthopaedic surgeon at the earliest







Comments